This article was updated on 23 July, 2022.
In Australia in 2022 it is the middle of winter and we now face a third Covid-19 wave. We have already had more deaths from Covid this year than the two years put together.
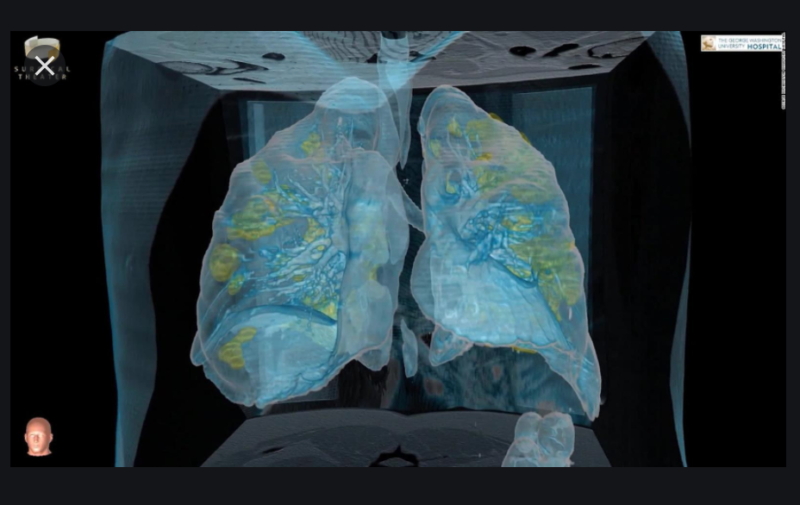
So it’s worth revisiting our article on Acute Respiratory Distress Syndrome (ARDS) and let’s begin with this short animation on what it looks like.
This video shows the progression of diffuse alveolar damage which is thought to be underlying the cause of Acute Respiratory Distress Syndrome. Read on.
Science papers coming in are confirming the quite different acute respiratory distress syndrome (ARDS) of Covid-19 patients, compared to the usual. It’s morbid, we know. But being educated in how different deaths can be, will help us navigate our own – and help us to support others as they face theirs.
So back to that science. It’s unusual to see such a speedy deterioration in the capacity to draw oxygen deep into the lungs, and therefore to oxygenate the blood supply, while the lungs appear to be normal.
Patients who’ve been in something like a car accident or ingested caustic soda, are usually the ones who have this unusual, rapid, onset of acute respiratory distress. But in Covid-19 cases it’s happening about a little over a week after the first signs of infection, then when it develops, overwhelming the patient very quickly.
The New York Times prepared a very good video of this in 2020 and two papers released at a similar time back up the theory about the unique features of ARDS.
Here is a paraphrasing of some of the points made, (but not all) in a paper submitted online on 24 April, to the Medical Journal of Australia (MJA).
- ARDS develops in 42 per cent of patients presenting with Covid-19 pneumonia, and 61-81% of those requiring ICU care.
- Covid-19 ARDS follows a predictable time course over days, with a median time to the need to insert tubing into the airways, to help with breathing, of about 8.5 days after symptoms start.
The MJA paper said: “ARDS causes diffuse alveolar damage in the lung. There is hyaline membrane formation in the alveoli in the acute stage, and this is followed by interstitial widening and by edema and then fibroblast proliferation in the organizing stage.”
This means the lining of the tiny sacs in the lungs where the exchange of oxygen takes place is damaged and a layer of debris forms that stops the oxygen exchange. In this process fluid forms and builds up, stopping the patient from being able to draw oxygen from the lungs into the blood supply.
This article is available at: https://www.mja.com.au/journal/2020/covid-19-ards-clinical-features-and-differences-usual-pre-covid-ards
Covid-19 pneumonia also appears to have unique features. For the scientifically minded, an Italian team involved with Covid-19 patients has reported on this. They also observe that the patient can have ARDS even though the lungs seem to be normal.
For their article, go to Covid-19 pneumonia: different respiratory treatments for different phenotypes by Luciano Gattinoni and others published by the American Thoracic Society at: https://link.springer.com/article/10.1007/s00134-020-06033-2
Each death is different. But the cause will determine the lead up. To read about natural death from old age, go to: https://good-grief.com.au/is-death-painful-or-more-like-uncomfortable/
CPR is done to avoid a death from heart failure, although the dynamics of this may have changed under Covid-19 hospital conditions. To read about the way CPR (cardiopulmonary resuscitation), is normally managed, go to:https://good-grief.com.au/why-cpr-is-often-not-compatible-with-a-quiet-death/
For the challenges to managing CPR in Covid-19 A&E conditions, go to:https://good-grief.com.au/lets-avoid-collateral-damage/
